Abstract
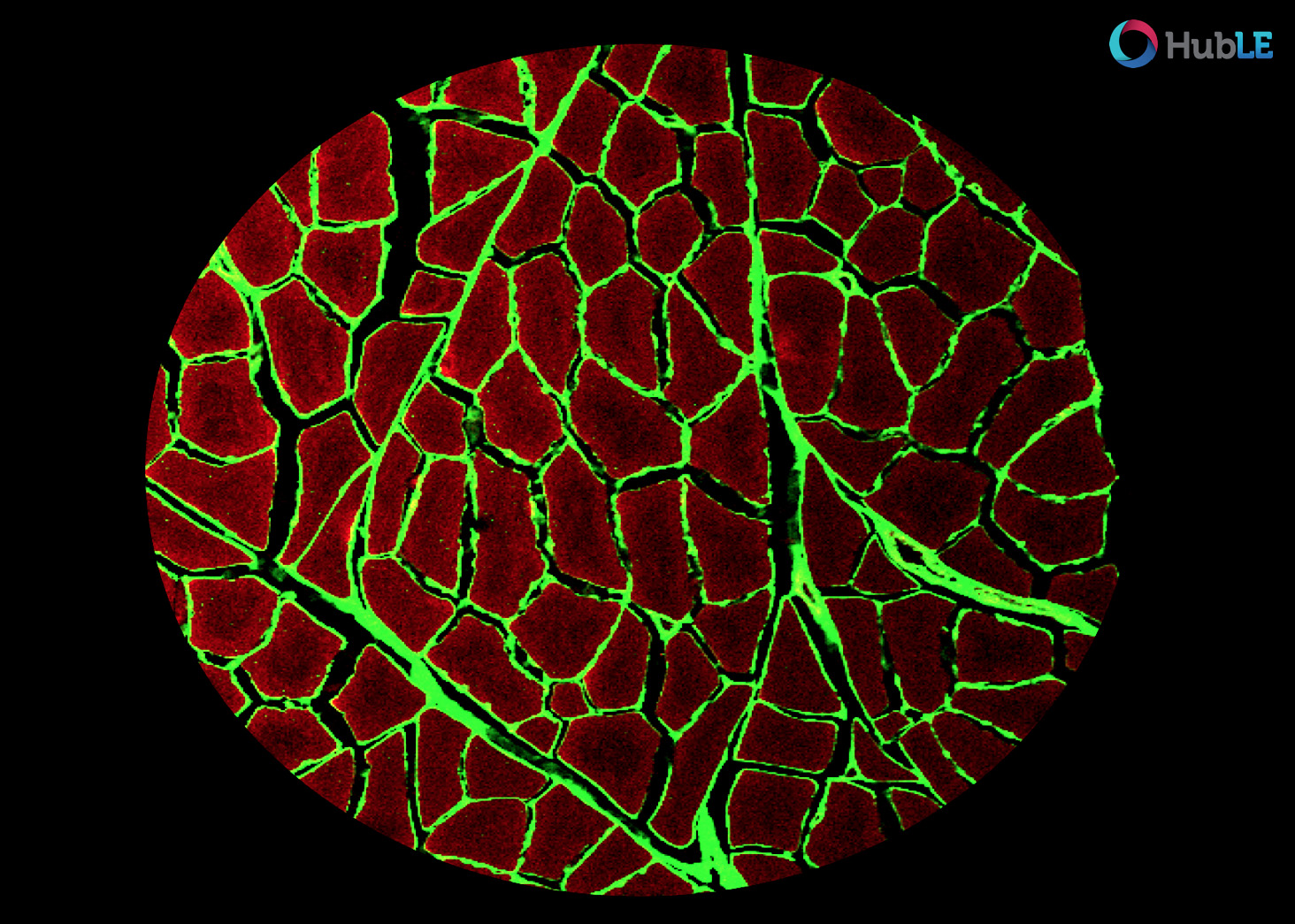
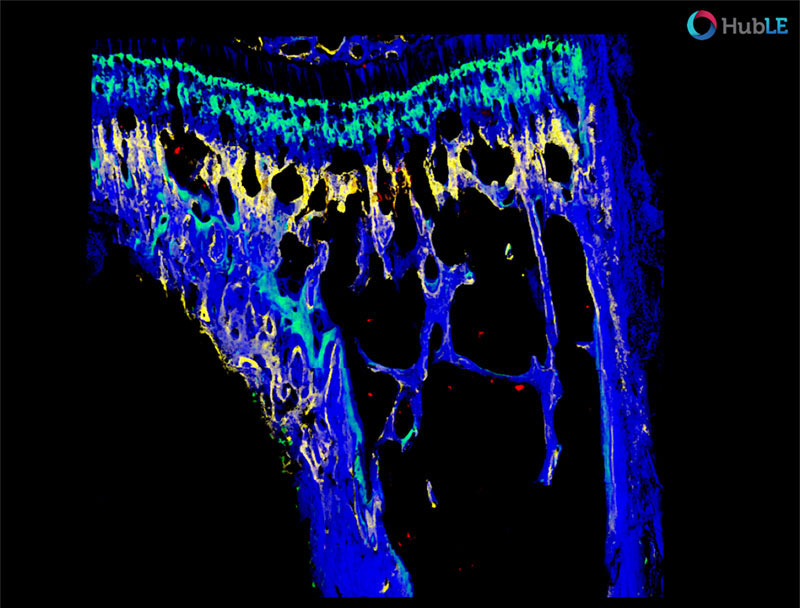
The pericellular matrix (PCM) of cartilage is a structurally distinctive microdomain surrounding each chondrocyte, and is pivotal to cell homeostasis and cell-matrix interactions in healthy tissue. This study queried if the PCM is the initiation point for disease or a casualty of more widespread matrix degen- eration. To address this question, we queried the mechanical properties of the PCM and chondrocyte mechanoresponsivity with the development of post-traumatic osteoarthritis (PTOA). To do so, we inte- grated Kawamoto’s film-assisted cryo-sectioning with immunofluorescence-guided AFM nanomechanical mapping, and quantified the microscale modulus of murine cartilage PCM and further-removed extracel- lular matrix. Using the destabilization of the medial meniscus (DMM) murine model of PTOA, we show that decreases in PCM micromechanics are apparent as early as 3 days after injury, and that this pre- cedes changes in the bulk ECM properties and overt indications of cartilage damage. We also show that, as a consequence of altered PCM properties, calcium mobilization by chondrocytes in response to me- chanical challenge (hypo-osmotic stress) is significantly disrupted. These aberrant changes in chondro- cyte micromechanobiology as a consequence of DMM could be partially blocked by early inhibition of PCM remodeling. Collectively, these results suggest that changes in PCM micromechanobiology are lead- ing indicators of the initiation of PTOA, and that disease originates in the cartilage PCM. This insight will direct the development of early detection methods, as well as small molecule-based therapies that can stop early aberrant remodeling in this critical cartilage microdomain to slow or reverse disease progression.
Article
Full text of Dr D. Chery’s article is available from HERE